By Scott Froum, DDS
Peri-implantitis is an inflammatory process affecting the soft and hard tissues surrounding an implant. This disease is associated with loss of supporting bone, bleeding on probing, and occasionally suppuration. The etiopathogenesis of peri-implantitis is complex and related to a variety of factors that affect the peri-implant environment. Peri-implantitis can be influenced by three factors:
- Patient-related factors including systemic diseases (e.g, diabetes, osteoporosis) and prior dental history (periodontitis)
- Social factors such as inadequate oral hygiene, smoking, and drug abuse
- Parafunctional habits (bruxism and malocclusion).
In addition to the above, iatrogenic factors such as faulty restorations, cement left following restoration delivery, and/or loose components can also play a significant role in the development of peri-implantitis.
Although restorations of endosseous implants have demonstrated a very high survival rate1, one study suggested that over a five-year period, 0 to 14.4% of dental implants demonstrated peri-implant inflammatory reactions associated with crestal bone loss.2
Many methods of treating peri-implantitis have been documented in the literature and most focus on removal of the contaminating agent from the implant surface. These treatments include:
- Administration of systemic antibiotics alone
- Mechanical debridement with or without systemic antibiotic treatment3
- Mechanical debridement with or without localized drug delivery and chlorhexidine oral rinses3a
- Mechanical debridement combined with LASER decontamination4
- Surgical debridement, and more recently …
- Surgical debridement with guided bone regeneration (GBR) for reparation of bony and soft-tissue defects.5
To date, GBR using a bone graft and membrane has had the best success as in demonstrating bone fill of the defects associated with peri-implantitis as described in the literature.6
Because there are biologic differences between teeth and implants, the progression of infection around implants is different than natural teeth. The inflammatory cell infiltrate around implants was reported to be larger and extend more apically when compared to a corresponding lesion in the gingival tissue around natural teeth. In addition, the tissues around implants are more susceptible to plaque-associated infections that spread into the alveolar bone.7
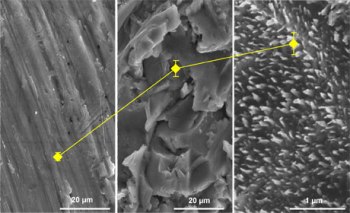
Implant surface bacterial decontamination is essential in treating peri-implantitis infections. Systemic administration of antibiotics has been used in the treatment of peri-implantitis, resulting in a reduction of inflammation. However, the efficacy of antibiotic therapy as a sole therapy has limited efficacy due to bacterial recolonization of the implant surface.8
Because nonsurgical treatment approaches failed to promote the reosseointegration of the exposed implant sites,9additional surgical interventions have been used in order to minimize the risk for a reinfection of the peri-implant pocket. Some of the treatment modalities suggested for peri-implantitis are:
- Mechanical/ultrasonic debridement with localized drug delivery; i.e., antimicrobial minocycline spheres (Arestin®)
- Laser treatment with and without flap access
- Open flap debridement
- Open flap debridement with guided bone regeneration
Renvert et al. (2006) compared the combination of mechanical debridement and topical application of minocycline microspheres to the combination of mechanical debridement and 1% chlorhexidine gel application in peri-implant lesions. The results obtained after a follow-up period of 12 months showed that with the chlorhexidine group, only a limited reduction in bleeding on probing was achieved and the mean peri-implant probing depth (PD) remained unchanged (3.9 mm). On the other hand, in the minocycline group, the reduction of bleeding on probing was greater and an improvement in mean peri-implant PD (from 3.9 mm to 3.6 mm) was seen. These results suggest that the topical application of chlorhexidine provides limited or no adjunctive clinical improvement when treating shallow peri-implant lesions as compared with using mechanical debridement alone.10
Schwarz et al. (2005, 2006a) compared the efficacy of the Er:YAG laser with that of the combination of mechanical debridement (using plastic curettes) and antiseptic (0.2% chlorhexidine digluconate) administration for the treatment of peri-implantitis. In both studies, the results obtained six months after therapy suggested that the treatment modalities were equally effective in improving peri-implant probing pocket depth (PPD) and clinical attachment level (CAL). However, at 12 months, the mean values for both groups of peri-implant PPD and CAL were not statistically significantly different from the corresponding values at baseline. Therefore, the results of the Er:YAG laser seem to be limited to a six-month period, particularly for advanced peri-implantitis lesions.
Leonhardt et al. evaluated the five-year outcome of a combined surgical (open flap) and antimicrobial treatment of peri-implantitis in humans. Leonhardt studied the effect of systemic antimicrobial therapy (amoxicillin and metronidazole) together with an open flap procedure and in conjunction with mechanical debridement of the implant surface for decontamination. The treatment was successful in 58% of the implants treated during follow-up for five years. Smoking was found to be a negative risk factor for treatment success.11
Schwarz et al. (2006b) evaluated and compared the efficacy of two bone regenerative procedures for the treatment of moderate intrabony peri-implantitis lesions that included a greater than 6 mm probing depth and an intrabony component of 3 mm as detected on radiographs. The defects were randomly treated either with a surgical debridement and filled with nanocrystalline hydroxyapatite, or surgical debridement and filled with bovine-derived xenograft (Bio-Oss®, Geistlich, Wolhusen, Switzerland) combined with a bioresorbable porcine-derived collagen membrane (Bio-Gide®, Geistlich, Wolhusen, Switzerland). After two years, the study showed that the combination of bovine bone mineral and the collagen membrane seemed to yield greater improvements in clinical parameters, showing 0.9 ± 0.2 mm more in PD reduction and 1.0 ± 0.3 more clinical attachment gain.12,13
Conclusion
The ideal management of peri-implant infections should focus both on infection control of the lesion, detoxification of the implant surface, and regeneration of lost support. Treatment options can be surgical or nonsurgical. To date, studies suggest that nonsurgical treatment of peri-implantitis is unpredictable, and the use of chemical agents such as chlorhexidine has only limited effects on clinical and microbiological parameters. Adjunctive local or systemic antibiotics have shown to reduce bleeding on probing and probing depths in combination with mechanical debridement. Beneficial effects of laser therapy on peri-implantitis have been shown, but this approach needs to be further evaluated. Implant surface bacterial decontamination is essential in treating peri-implantitis infections. Most studies suggest that establishing an adequate healthy peri-implant tissue environment proves to be difficult since inflammation is still present in a significant number of patients. New treatment modalities need to be evaluated using long-term randomized-controlled studies to identify predictable and successful treatment of peri-implantitis.
Author bio
Scott Froum, DDS, is a periodontist and co-editor of Surgical-Restorative Resource e-newsletter. He is a clinical associate professor at the New York University Dental School in the Department of Periodontology and Implantology. He is in private practice in New York City. You may contact him by email at drscottfroum@yahoo.com.
References
1. Albrektsson T et al. Osseointegrated oral implants — A Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol 1988;5 9:287-296.
2. Berglundh T et al. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol 2002; 29:197-212.
3. Renvert S. (2008), Nonsurgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol. Sept. 2008; 35(8 Suppl):305-315.
3a. Rosenberg ES et al. Microbial differences in two clinically distinct types of failures of osseointegrated implants. Clin Oral Implants Res 1991; 2:135-144.
4. Schwarz F et al. (2006a). Nonsurgical treatment of moderate and advanced peri-implantitis lesions: a controlled clinical study. Clinical Oral Investigations 10, 279–288.
5. Klinge B et al. A systematic review of the effect of anti-infective therapy in the treatment of peri-implantitis. J Clin Periodontol 2002; 29:213-220.
6. Grunder U et al. Treatment of ligature-induced peri-implantitis using guided tissue regeneration: a clinical and histologic study in the beagle dog. Int J Oral Maxillofac Implants 1993; 8:282-292.
7. Lindhe J et al. (1992). Experimental breakdown of peri-implant and periodontal tissues. Clin Oral Impalnts Res 1992; 3:9-16.
8. Mombelli A, Lang NP. Antimicrobial treatment of peri-implant infections. Clin Oral Implants Res 1992; 3:162-168.
9. Schwarz F et al. (2006). Influence of different treatment approaches on nonsubmerged and submerged healing of ligature-induced peri-implantitis lesions: an experimental study in dogs. Journal of Clinical Periodontology Aug. 2006; 33(8):584-595.
10. Renvert S. Topical minocycline microspheres versus topical chlorhexidine gel as an adjunct to mechanical debridement of incipient peri-implant infections: a randomized clinical trial. J Clin Periodontol. May 2006; 33 (5): 362-369.
11. Leonhardt A. (2003). Five-year clinical, microbiological, and radiological outcome following treatment of peri-pmplantitis in man. J Periodontol 2003; 74:1415-1422.
12. Schwarz F et al. (2006b). Healing of intrabony peri-implantitis defects following application of a nanocrystalline hydroxyapatite (Ostim®) or a bovine-derived xenograft (Bio-Oss) in combination with a collagen membrane (Bio-Gide). A case series. Journal of Clinical Periodontology 33; 491–499.
13. Schwarz F et al. (2008). Two-year clinical results following treatment of peri-implantitis lesions using a nanocrystalline hydroxyapatite or a natural bone mineral in combination with a collagen membrane. Journal of Clinical Periodontology 35; 80–87.